Translate this page into:
Early complications of anterior cervical discectomy and fusion: A case series
2 Department of Neurosurgery, Almustansiriyah College of Medicine, Baghdad, Iraq
3 Department of Orthopedics, Spine Surgeon Baquba Teaching Hospital, Baghdad, Iraq
4 Department of Orthopedics, Ahrar Specialist Hospital, Zagazig, Cairo, Egypt
Corresponding Author:
Ghazwan A Hasan
Jadria Private Hospital, Baghdad
Iraq
dr.bayaty@gmail.com
| How to cite this article: Hasan GA, Raheem HQ, Al-Naser LM, Sheta RA. Early complications of anterior cervical discectomy and fusion: A case series. J Musculoskelet Surg Res 2018;2:121-125 |
Abstract
Objectives: Anterior cervical discectomy and fusion (ACDF) is a common procedure in cervical degenerative disorders and cervical trauma patients. However, this procedure and approach are associated with peri- and post-operative complications. This study aims to report peri- and early postoperative complications occurred during ACDF and also tries to find any relation between dysphagia and plating, smoking, or age. Methods: This is a multicentric prospective study conducted on 165 patients; 116 males (70.3%) and 49 females (29.7%); their age range was 33—61 years (mean age, 42.5 years). The study started from January 2013 to February 2017. The follow-up was for 6 weeks, and we evaluated the clinical and radiographic signs of complications. Results: Fifty-seven patients (34.5%) had transient dysphagia and two patients (1.2%) each had a dural tear, surgical-site infection, and postoperative hematoma. One patient (0.6%) each had an esophageal injury, slippage of the cage, Brown—Sequard syndrome, acute implant extrusion, and Horner syndrome. No patient had a recurrent laryngeal nerve injury. The risk factors for dysphagia include female sex, multilevel surgery, plating, and smoking, most of the dysphagic symptoms were mild in severity and lasted <6 weeks. Conclusion: Not all complications of ACDF require surgical intervention, and most of them could be treated nonoperatively with careful follow-up. Our results are comparable with what was reviewed in the literature. The incidence of complications is increased with more than one-level fusion and in multiple comorbid disorders (including diabetes mellitus and smoking). Most of the postoperative dysphagic symptoms are mild and last <6 weeks.Introduction
Cervical degenerative disc disease (DDD) is a common problem in spine practice, and most of the cervical disc herniation cases are treated conservatively, and surgery is an indication in the failure of conservative treatment or in patients having a neurological deficit. Anterior cervical discectomy and fusion (ACDF) is the gold standard surgical procedure for the management of symptomatic cervical DDD.[1],[2] This approach was introduced by Smith, Robinson, and Cloward in 1958.[2],[3] Initially, they used the harvested iliac crest as a method of fusion, but with a high rate of donor-site morbidity and subsidence, they shifted toward synthetic cage (either a polyetheretherketone [PEEK] cage or titanium).[4],[5],[6] The approach uses natural planes to reach the cervical spine and therefore is considered less traumatic. However, this procedure has been associated with peri- and postoperative complications[4] such as a postoperative hematoma, esophageal injury, vascular injury, dysphagia, and vocal cord paresis, which can be potentially debilitating or life-threatening.[5],[7],[8],[9],[10],[11],[12],[13],[14],[15] It has been found that most of the complications are underreported in the literature, even in sizeable clinical case series.[6],[9] Therefore, the awareness, expectation, and prediction of these complications beforehand is mandatory for good outcome after this operation. This study aims to report peri-operative and early postoperative complications occurred during ACDF and also tries to find any relation between dysphagia and plating, smoking, or age.
Materials and Methods
A prospective multicentric case series study was performed from January 2013 to February 2017 in four centers in Baghdad, Iraq. This study started with 170 cases, which fulfilled the inclusion criteria. Three cases were missed in the 2-week follow-up, and another two cases missed their 6-week appointment. One case died secondary to esophageal injury, which was involved in the study as a complication. The remaining 165 cases were the substance of the study with complete follow-up.
All patients met the inclusion criteria, which include single-, two-, or three-level DDD, with a failure of conservative management. Presenting symptoms were radiculopathy or myelopathy, in which the primary pathology was anterior and underwent ACDF. The exclusion criteria were cervical tumors, cervical trauma, revision surgery, myelopathy with ossification of posterior longitudinal ligaments, myelopathy with stenotic pathology from posterior, which need posterior surgeries, previous neck surgery as thyroidectomy. All patients in this study were treated surgically by ACDF with or without plating.
Intra- and post-operative complications were noted in each patient. Follow-up of the patients was performed for 3 months. Dysphagia is classified according to Bazaz Dysphagia Score[16] into none, mild, moderate, and severe. The transient dysphagia item is used when dysphagia lasts >2 weeks and <1 month.
Under general anesthesia, a left-sided anterior Smith—Robinson approach was used. Anterior cervical discectomy using a high-speed drill, surgical loops, and disc rongeur was performed. A PEEK cage was used for single-level cases and some of the two-level cases, while plating was used in three-level cases and some of the two-level cases. Postoperatively, anteroposterior and lateral radiographs were ordered, and removal of sutures was done after 10 days. Postoperatively, a soft collar was worn for 12 weeks in all cases.
Results
We recruited 165 patients in our study including 119 males (70.3%) and 49 females (29.7%) with a male:female ratio of 5:2 [Table - 1]. The age of our patients ranged from 33 to 61 years, with the typical age of presentation between 30 and 50 years in >70% of cases (mean age was 44 years and standard deviation was 10.39) [Table - 1].
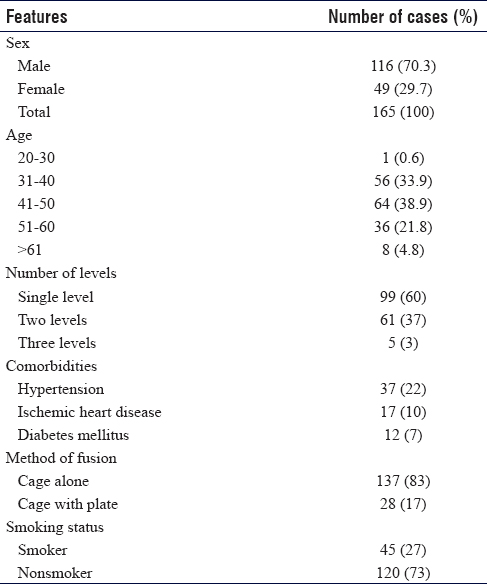
We had 236 levels involved in the surgery, which was distributed from C3—C4 to C6—C7, in which C5—C6 was the most common level operated (100 cases, 42.3%) [Table - 1].
The comorbidities in our cases were as follows hypertension in 37 cases (22%), ischemic heart disease in 17 cases (10%), and diabetes mellitus (DM) in 12 cases (7%) [Table - 1].
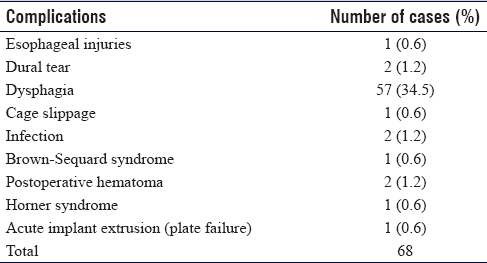
The method of fusion was cage alone in 137 cases (83%), while cage with plating was used in 28 cases (17%) [Table - 1].
We observed the intra- and post-operative complications, and they were as follows: dysphagia in 57 cases (34.7%), a dural tear in two cases (1.2%), postoperative hematoma in two cases (1.2%), and postoperative wound infection in two cases (1.2%). An esophageal injury, Horner syndrome, cage migration, acute implant extrusion (plate failure), and Brown—Sequard syndrome each in one case (0.6%) [Table - 2].
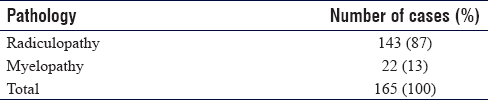
The presenting symptoms of our cases were radiculopathy in 143 cases (87%), while myelopathy in 22 cases (13%) [Table - 3].
We had 99 cases with single-level surgery (60%), 61 cases with two-level (37%), and only 5 cases with three-level surgery (3%) [Table - 4].

We observed the underlying conditions in dysphagia patients' group, and we found that the most common risk factors were plating (71% of plating cases developed dysphagia), while 64% of multi-level surgery patients developed dysphagia and 51% of smokers and 40% of females developed dysphagia with other risk factors as summarized in [Table - 5].

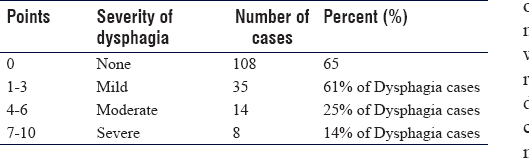
According to Bazaz scoring scale,[16] we found that 35 dysphagia cases were mild (61%), while 14 cases had moderate dysphagia (25%) and eight cases had severe dysphagia (14%) [Table - 6].
Discussion
ACDF is an apprising procedure that can be considered to relieve the compression, restore the alignment, stabilize the spine, and decrease the pain in cervical spine pathology. In the current study, the majority of operated patients (87%) had radiculopathy, with only 13% of them having myelopathy.
Most of the patients (65.5%) were more than 40 years of age, which is expected because the degenerative disease of the spine including cervical spine is more common in middle and old age groups.
It is suggested that degenerative cervical spine is more common in males than females as 70.3% were males in our study. Radiculopathy and myelopathy are more common in males than females, which is compatible with what is published in the literature.[17] This could be because of the dominance of males in the family and related to heavy work that males do or could be due to smoking, which is more common in males and is a risk factor for DDD.[17]
The follow-up data collection timing of our patients was intraoperative, postoperative day 1, 10 days (time for suture removal), 6 weeks, and 3 months.
The most common complication encountered in our study was transient painful dysphagia, which occurred in about 34.5% of cases (57/165 patients). The term of transient dysphagia is defined as painful dysphagia for >2 weeks but <1 month. Most of our dysphagia cases presented with mild transient dysphagia (61%) according to BAZAZ score.[16] Compared to Pan et al.[18] who reported the incidence of postoperative dysphagia as 32%, Bazaz et al. reported[16] the incidence of 50.2% of dysphagia at 1 month.
When we reviewed the risk factors of dysphagia, we found that the incidence in patients above 60 years of age was 62% (5/8 of cases), 40% in females, 50% in patients with comorbidities, and 64% in multi-level surgery. These findings are similar to what is seen in the previous studies of Riley et al. and Kalb et al.[19],[20] In the current study, the incidence of dysphagia in smokers was 51%, which is higher than the nonsmoker group (28%); again these findings are similar to what is in a previous study by Olsson et al.[21] Dysphagia may result from a prolonged traction of the esophagus by retractors during surgery, in multi-level surgery, or in using a plate with cages. In our study, the results look lower in comparison to that mentioned in the literature partially due to the fact that most of our cases were single-level surgery, or most of our cases were treated with cage alone without a plate. There are few studies supporting the use of intravenous steroids to decrease the risk of dysphagia as in Siasios et al., although in the same study they found that steroid may interfere with fusion.[22] Pan et al.[18] recommended that the use of intermittent retracting with temporary relief of the pressure on the esophagus seems to reduce the incidence of postoperative dysphagia.
The incidence of intraoperative dural tears in our study was 1.2% (2/165 patients), and this occurred in a 59-year-old male patient, who was diabetic and smoker and presented with a C5—C6 and C6—C7 DDD and cervical myelopathy, and in a 62-year-old patient with two-level stenosis and calcification of the discs. The tear occurred while we were trying to remove the posterior osteophyte from the vertebral body and they were small tears of about 1 mm, and we left them without repair and the insertion of the cage was done in both cases. Close postoperative follow-up was practiced, and no further complications were noticed during the postoperative period in both cases. On reviewing the literature, the incidence of dural tears in cervical spine surgery is about 1%, which is comparable to our study, and this agrees with Hannallah et al.[23] for; the dural tears were more with the use of rongeurs.
In this study, we faced two patients (1.2%) who developed a postoperative hematoma and presented with neck pain and dysphagia. The first case was a 56-year-old patient with DDD of C5—C6, who had ACDF, hemostasis was secured and, 24 h postoperatively, he developed swelling in the neck with mild dyspnea and dysphagia. His clinical evaluation revealed a swelling in the anterior neck. Drainage of hematoma through the surgical incision site was done and the patient was kept in hospital for another 2 days for close follow-up and was discharged well. The second patient was a 49-year-old female who was operated for C5—C6, and C6—C7 fusion and plating, she developed a swelling in the neck 8 h postoperatively and a nonfunctioning drain was discovered. Direct drainage of the hematoma with close follow-up was performed and the patient was discharged on the 3rd postoperative day in good condition. In the review of the literature, the reported incidence of this complication has varied from 0.2% to 1.9%.[14] Hematoma may be the result of inadequate control of arterial or venous bleeding during the operation and has been reported due to superior thyroid artery dissection.[15]
Migration of the cage was seen in one patient (0.6%) out of all cases. The patient was a 58-year-old male presented with DDD of C5—C6 with myelopathy changes. On the 3rd postoperative day, he had an accidental movement of his neck without collar support, which was followed by dysphagia. Radiographically, there was an anterior migration of the cage [Figure - 1]. He was managed conservatively using rigid collar support and did not require revision of surgery as the symptoms were relieved consequently. Most studies have shown that swallowing problem tends to resolve with time. In the review of the literature, dysphagia is the most common presenting symptom, and the incidence of slippage varies from 3% to 14%.[24] Using the new techniques, which have a rigid fixation and higher stability such as PEEK cage, may help lower the incidence of this complication.
 |
| Figure 1: Cervical disc C4�C5, which subsided on final follow-up and managed conservatively |
There was one patient with an esophageal injury in our study (0.6%) occurred in a 56-year-old female with C5—C6, and C6—C7 ACDF 3 days postoperatively, the patient developed pain, dysphagia, fever, and progression of symptoms. Further investigation by barium swallow revealed leakage of dye. Diagnosis of esophageal injury was confirmed, admission to the hospital and exploration was done by a head-and-neck surgeon who repaired the defect with modified muscle flap, but the patient died 2 days later due to complicated mediastinitis. In the review of the literature, the incidence of esophageal injuries is about 0.02%—1.52%, which is same as in our study. Diagnosis of the tear could be intraoperative, early postoperative (as in our case), or late postoperative period.[25] The common causes of the tear are erosions by hardware, trauma, or intraoperative iatrogenic injury, as in our case.[25],[26]
One patient was discovered to have Horner syndrome (0.6%) postoperatively. He was a 48-year-old male presented with features of Horner syndrome; it was transient in nature, and complete resorption of symptoms occurred within 4 weeks following conservative treatment. In a review of the literature, the incidence is ranging between 0.1% as in Fountas et al.,[9] and 1.1% as in Bertalanffy and Eggert,[7] and the treatment was the same as in previous literature. Knowing the anatomical relationship between the longus coli muscle and the sympathetic trunk, the use of subperiosteal dissection and placing the retractors under the medial edge of the longus coli are recommended to avoid this complication.[27]
Another patient was diagnosed with superficial wound infections (0.6%); a 54-year-old female, diabetic, who was operated for two-level myelopathy, i.e. C4—C5 and C5—C6 and, on the 6th postoperative day, she had pain at the site of the wound and induration with redness. She was treated conservatively by close follow-up, control of her blood sugar and an oral antibiotic. In the literature, the incidence is ranging between 0.3% and 3%.[5],[8],[27]
The infection is ranging from superficial soft-tissue wound infections, deep wound infection, discitis to prevertebral abscess. Good preoperative control of risk factors, following the guidelines of sterilizations, and meticulous soft-tissue dissection and good hemostasis, are recommended to prevent or minimize the infection.
There was also one case of neurological complication (0.6%) as a Brown—Sequard syndrome. A 40-year-old male had ACDF for C5—C6, presented immediately postoperatively with right hemiparesis and left-sided sensory impairment, especially in the area below the first thoracic vertebra level. Immediate magnetic resonance imaging was done which revealed cord contusion. He was managed with close follow-up and physiotherapy till resorption of symptoms, which took 3 months. Neurological complications are rare; they are critical complications following ACDF. The incidence in the literature is 0.88%—5.4%.[7],[11],[27],[28],[29] In our case, we faced a Brown—Sequard syndrome, which is rare with no previous similar cases reported in the literature.
We had one case (0.6%) of acute implant extrusion in a 64-year-old female with a history of multilevel cervical DDD and osteoporosis presented with myelopathy. The patient presented with increasing severity of dysphagia after 2 weeks of surgery. The radiograph showed mild extrusion of the implant with displacement in the coronal plane. She was treated with extended cervical collar and close follow-up, and there was no need for revision surgery. In the literature, the rate of acute implant extrusion is ranging between 0% and 0.8%; it occurred in the first 30 days in most cases. It occurs mainly in elderly patients with degenerative cervical spine and osteoporosis. The decision of treatment is ranging from conservative to revision and posterior stabilization.
Conclusion
Not all complications require surgical intervention, and most of them could be treated nonoperatively with careful follow-up. Our results are comparable with what reviewed in the literature. The incidence of complications increased with more than one level of fusion and in multiple comorbid disorders (including DM and smoking). Dysphagia was the most common complication, and in most of the cases, it was mild and lasted <6 weeks. Multilevel surgery, using a plate, smoking, and female gender were the factors that increased the risk of dysphagia.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Authors' contributions
All authors' have equal contribution's in each part of this paper including surgery and paper preparations. All authors have critically reviewed and approved the final draft and are responsible for the content and similarity index of the manuscript.
| 1. | Amhaz HH, Kuo R, Vaidya R, Orlewicz MS. Esophageal perforation following cervical spine surgery: A review with considerations in airway management. Int J Crit Illn Inj Sci 2013;3:276-8. [Google Scholar] |
| 2. | Cloward RB. The anterior approach for removal of ruptured cervical disks. J Neurosurg 1958;15:602-17. [Google Scholar] |
| 3. | Smith GW, Robinson RA. The treatment of certain cervical-spine disorders by anterior removal of the intervertebral disc and interbody fusion. J Bone Joint Surg Am 1958;40-A: 607-24. [Google Scholar] |
| 4. | Yang SY, Lee SB, Cho KS. Delayed esophagus perforation after anterior cervical spine surgery. Korean J Neurotrauma 2015;11:191-4. [Google Scholar] |
| 5. | Burke JP, Gerszten PC, Welch WC. Iatrogenic vertebral artery injury during anterior cervical spine surgery. Spine J 2005;5:508-14. [Google Scholar] |
| 6. | Morpeth JF, Williams MF. Vocal fold paralysis after anterior cervical diskectomy and fusion. Laryngoscope 2000;110:43-6. [Google Scholar] |
| 7. | Bertalanffy H, Eggert HR. Complications of anterior cervical discectomy without fusion in 450 consecutive patients. Acta Neurochir (Wien) 1989;99:41-50. [Google Scholar] |
| 8. | Flynn TB. Neurologic complications of anterior cervical interbody fusion. Spine (Phila Pa 1976) 1982;7:536-9. [Google Scholar] |
| 9. | Fountas KN, Kapsalaki EZ, Nikolakakos LG, Smisson HF, Johnston KW, Grigorian AA, et al. Anterior cervical discectomy and fusion associated complications. Spine (Phila Pa 1976) 2007;32:2310-7. [Google Scholar] |
| 10. | Gaudinez RF, English GM, Gebhard JS, Brugman JL, Donaldson DH, Brown CW, et al. Esophageal perforations after anterior cervical surgery. J Spinal Disord 2000;13:77-84. [Google Scholar] |
| 11. | Lied B, Sundseth J, Helseth E. Immediate (0-6 h), early (6-72 h) and late (>72 h) complications after anterior cervical discectomy with fusion for cervical disc degeneration; discharge six hours after operation is feasible. Acta Neurochir (Wien) 2008;150:111-8. [Google Scholar] |
| 12. | Lu DC, Tumialán LM, Chou D. Multilevel anterior cervical discectomy and fusion with and without rhBMP-2: A comparison of dysphagia rates and outcomes in 150 patients. J Neurosurg Spine 2013;18:43-9. [Google Scholar] |
| 13. | Riley LH Jr., Robinson RA, Johnson KA, Walker AE. The results of anterior interbody fusion of the cervical spine. Review of ninety-three consecutive cases. J Neurosurg 1969;30:127-33. [Google Scholar] |
| 14. | Tew JM Jr., Mayfield FH. Complications of surgery of the anterior cervical spine. Clin Neurosurg 1976;23:424-34. [Google Scholar] |
| 15. | Yu NH, Jahng TA, Kim CH, Chung CK. Life-threatening late hemorrhage due to superior thyroid artery dissection after anterior cervical discectomy and fusion. Spine (Phila Pa 1976) 2010;35:E739-42. [Google Scholar] |
| 16. | Bazaz R, Lee MJ, Yoo JU. Incidence of dysphagia after anterior cervical spine surgery: A prospective study. Spine (Phila Pa 1976) 2002;27:2453-8. [Google Scholar] |
| 17. | Chatley A, Kumar R, Jain VK, Behari S, Sahu RN. Effect of spinal cord signal intensity changes on clinical outcome after surgery for cervical spondylotic myelopathy. J Neurosurg Spine 2009;11:562-7. [Google Scholar] |
| 18. | Pan YH, Cheng CY, Chen SY, Lin JF, Chiou TL, Chen WF, et al. Complications of multilevel anterior cervical fusion. Tzu Chin Med J 2004;16:79-83. [Google Scholar] |
| 19. | Riley LH 3rd, Skolasky RL, Albert TJ, Vaccaro AR, Heller JG. Dysphagia after anterior cervical decompression and fusion: Prevalence and risk factors from a longitudinal cohort study (presented at the 2004 CSRS Meeting). Spine 2005;30:2564-9. [Google Scholar] |
| 20. | Kalb S, Reis MT, Cowperthwaite MC, Fox DJ, Lefevre R, Theodore N, et al. Dysphagia after anterior cervical spine surgery: Incidence and risk factors. World Neurosurg 2012;77:183-7. [Google Scholar] |
| 21. | Olsson EC, Jobson M, Lim MR. Risk factors for persistent dysphagia after anterior cervical spine surgery. Orthopedics 2015;38:e319-23. [Google Scholar] |
| 22. | Siasios I, Fountas K, Dimopoulos V, Pollina J. The role of steroid administration in the management of dysphagia in anterior cervical procedures. Neurosurg Rev 2018;41:47-53. [Google Scholar] |
| 23. | Hannallah D, Lee J, Khan M, Donaldson WF, Kang JD. Cerebrospinal fluid leaks following cervical spine surgery. J Bone Joint Surg Am 2008;90:1101-5. [Google Scholar] |
| 24. | Jones J, Yoo J, Hart R. Delayed fracture of fibular strut allograft following multilevel anterior cervical spine corpectomy and fusion. Spine (Phila Pa 1976) 2006;31:E595-9. [Google Scholar] |
| 25. | Halani SH, Baum GR, Riley JP, Pradilla G, Refai D, Rodts GE Jr, et al. Esophageal perforation after anterior cervical spine surgery: A systematic review of the literature. J Neurosurg Spine 2016;25:285-91. [Google Scholar] |
| 26. | Li Y, Shen H, Khan KZ, Fang S, Liao Z, Liu W, et al. Comparison of multilevel cervical disc replacement and multilevel anterior discectomy and fusion: A systematic review of biomechanical and clinical evidence. World Neurosurg 2018. pii: S1878-8750(18)30957-4. [Google Scholar] |
| 27. | Yasumoto Y, Abe Y, Tsutsumi S, Kondo A, Nonaka S, Ito M, et al. Rare complication of anterior spinal surgery: Horner syndrome. No Shinkei Geka 2008;36:911-4. [Google Scholar] |
| 28. | Nanda A, Sharma M, Sonig A, Ambekar S, Bollam P. Surgical complications of anterior cervical diskectomy and fusion for cervical degenerative disk disease: A single surgeon's experience of 1,576 patients. World Neurosurg 2014;82:1380-7. [Google Scholar] |
| 29. | Kelly MP, Eliasberg CD, Riley MS, Ajiboye RM, SooHoo NF. Reoperation and complications after anterior cervical discectomy and fusion and cervical disc arthroplasty: A study of 52,395 cases. Eur Spine J 2018;27:1432-9. [Google Scholar] |
Fulltext Views
3,396
PDF downloads
391





