Translate this page into:
The association between attention deficit hyperactivity disorder and Legg–Calvé–Perthes disease in tertiary hospital-Riyadh City, Saudi Arabia
2 Department of Orthopedics, King Abdulaziz University Hospital, Jeddah, Saudi Arabia
3 College of Medicine, King Saud Bin Abdulaziz University for Health Sciences, Riyadh, Al Hars Al Watani, Ar Rimayah, Saudi Arabia
4 Department of Orthopedics, College of Medicine, King Khalid University, Abha, Saudi Arabia
Corresponding Author:
Mohammad A Almalki
College of Medicine, King Saud Bin Abdulaziz University for Health Sciences, Al Hars Al Watani, Ar Rimayah 14611, Riyadh, Saudi Arabia College of Medicine, King Saud Bin Abdulaziz University for Health Sciences, Riyadh
Saudi Arabia
mohammad_malki@hotmail.com
| How to cite this article: Al-Hunaishel MA, Almalki MA, Almaiman SS, Alqahtani TA, Alsaadi ZS, Aldosari BM, Al-Shehri SH. The association between attention deficit hyperactivity disorder and Legg–Calvé–Perthes disease in tertiary hospital-Riyadh City, Saudi Arabia. J Musculoskelet Surg Res 2018;2:156-160 |
Abstract
Objectives: Legg–Calvé–Perthes Disease (LCPD) is a juvenile hip disorder in which interruption to the blood supply of the femoral head causes osteonecrosis. Previous studies reported an association between attention deficit hyperactivity disorder (ADHD) and LCPD. This study aimed to assess the relationship between ADHD and LCPD disease in a tertiary hospital in Riyadh city, Saudi Arabia. Methods: This is a case–control study that included 50 case subjects (LCPD group) and 100 controls. Both groups underwent clinical assessment by the 5th edition of the Diagnostic and Statistical Manual of Mental Disorders criteria to diagnose ADHD and to compare the proportions in both groups. Results: The age range of the study population was 4–19 years. In the case group, we collected the data from 11 females and 39 males. The age ranged from 4 to 19 years (mean 9 years). While in the control group, we collected the data from 47 females and 53 males. The age range was 4–15 years (mean 8 years). In both groups, 34 children (22.7%) were diagnosed with ADHD, 15 (30%) in the case group and 19 (19%) in the control group. There was no significant difference in ADHD incidence between the case group and the control group (P = 0.1293, odds ratio = 1.827). LCPD has a significant male predominance (78%). Conclusions: We found that the prevalence of ADHD in LCPD is high (30%), which is comparable to the reported literature but as ADHD was higher than the reported literature in the control group (19%) the difference was statistically insignificant.
Introduction
Legg–Calvé–Perthes Disease (LCPD) is a juvenile hip disorder occurs secondary to blood supply interruption of the femoral head causing osteonecrosis. Over time, new blood vessels infiltrate the necrotic bone, and the tissue starts healing with a loss of bone mass and weakening of the femoral head.[1] It is estimated that the incidence of LCPD is from 4 to 290 in a million children younger than 15 years. Significant variability is found when considering the extent of LCPD within ethnic groups, and it is found to be more in lower socioeconomic classes. The classical age at presentation is usually around 4–8 years (average 6.5 years), except for children from the Indian subcontinent (average 9.5 years). The affected children exhibit slow bone maturation, mild short stature, reduced skeletal age, disproportionate growth, and low birth weight.[2] Patients with LCPD usually present with intermittent leg, thigh, and groin pain, which increases with movement. The diagnosis can be made with proper history taking, physical examination, and imaging studies.[1]
Attention deficit hyperactivity disorder (ADHD) is a neurodevelopmental syndrome. It has a continual pattern of impaired attention or inattention and hyperactivity-impulsivity that disrupt general well-being and functional development. It is usually diagnosed in childhood and may last through adulthood.[3] ADHD has three subtypes, which are the inattentiveness type, hyperactivity/impulsiveness, and the combined type.[3] Worldwide, ADHD affects about 5.3%–7.1% of children.[4] The prevalence of ADHD in Saudi Arabia has been investigated in multiple studies with a great variation in results. ADHD prevalence in Saudi Arabia was illustrated by Alqahtani who collected data of 708 primary school students in Saudi Arabia attending first to third school grades (7–9 years old), using the fourth Diagnostic and Statistical Manual of Mental Disorders (DSM-5) criteria of ADHD. The results showed that ADHD affected 2.7% of the sample. The prevalence was 2% for the inattention type, 1.4% for the hyperactive/impulsivity type, and 0.7% for the combined type.[5] In 2015, a study conducted in Riyadh city reported an 8.4% incidence of ADHD,[6] this conclusion is much higher compared to Alqahtani's study in Riyadh also, which reported a 2.7% incidence.[5] Furthermore, a third study done in 2013 conducted in Jizan city reported ADHD incidence of 13.5%,[7] this result was relatively close to another study conducted in 2013 in Jeddah city, which concluded that the incidence was 11.6%.[8] Also in 2012, a study conducted in Alkhobar city reported a 3.5% incidence, an important point to mention in this study is that it included only female school children.[9] In comparison, we found one study included only male school children that was conducted in Dammam city and it concluded an overall prevalence of combined ADHD of 16.4%.[10] Although this study reported a higher prevalence than the worldwide known prevalence of 3%–5%, it still carries good weight since the sample that was used has over 1200 males school students. One last study that we found worth reporting is a study conducted in 2016 in Abha. This study was done on school-age children who were born preterm and reported that the prevalence of ADHD among preterm children was high, with a result of 34% for the inattentive type and 11.3% for the hyperactive-impulsive type.[11]
There are multiple potential causes of ADHD including biochemical, genetics, physiological, and behavioral factors.[12] The multiple causes make the diagnosis of ADHD a complex matter. It requires a careful assessment of a number of specific symptoms in a variety of life settings. The fifth edition of the DSM-5 comprises criteria to diagnose ADHD. The criteria aim to unify standards between communities.[3] They clarified that people with ADHD show a continual pattern of inattention and hyperactivity-impulsivity that disrupts general well-being and functional development. The criteria consist of two domains of symptoms. The first one lists the symptoms of inattention, and the second one lists the symptoms of hyperactivity-impulsivity.
Based on the literature review, previous studies had highlighted that there is an association between ADHD and LCPD.[13],[14] In 1993, Loder et al. reported that there is a high incidence of ADHD among LCPD patients. The incidence was 33% compared to 3%–5% in the normal population.[13] Studying the relationship between ADHD and LCPD is important as ADHD prevalence in Saudi Arabia is high (16.4%) in Saudi males according to Al Hamed et al., when it is 5.3%–7.1% worldwide.[4],[10] The current study aims to investigate the relationship between ADHD and LCPD among young Saudi population.
Materials and Methods
A case–control study that involved 150 individuals was carried out. The sample size was 150 participants divided into two groups, a case group (LCPD patients) of 50 subjects and a control group (non-LCPD) of 100 subjects. The sample size was determined using 5% significance level, 80% power and 2:1 ratio of control to cases and an expected percentage of 15% ADHD incidence for the control group,[10] and an expected percentage of 35% ADHD incidence for case group.[13]
The case group included all Saudi cases diagnosed with LCPD between the ages of 4 and 19 years from both genders using the database of our institution. While the control group was chosen from the vaccination clinic (vaccinated children and their companions) to ensure that there is no medical reason for the hospital visit. Individuals under any psychiatric medication that influence the attention and activity were excluded from the study. The samples' age ranged from 4 to 19 years old. The minimum included age in our study was 4 years old, and the maximum was 19, this is due to the guideline of the American Academy of Pediatrics, which limits the age of diagnosing ADHD to 4–18 years old.[15] However, we included one LCPD case of 19 years old, as he was diagnosed long before that age, he was only seen at our hospital at 19.
Each subject in both groups was asked to visit the clinic for one time and undergo a clinical assessment, evaluation for ADHD, a detailed history was taken, and consents were obtained from the parents. Two instruments were used to collect data from children's parents from both groups. First, a data collection sheet that included demographical data such as date of birth, gender, height, and weight and the affected side in the case group. The other instrument measured the inattention and hyperactivity of both groups using the latest diagnosis criteria for ADHD by DSM-5, which was assessed by the researchers.[3]
After that, all collected data were coded into an Excel sheet and analyzed using SAS 9.4. Categorical data were described by frequencies and percentages, such as gender and affected side among LCPD patients, while numerical data were presented as a mean and standard deviation, such as age and body mass index (BMI). From the ADHD diagnostic test, any child who scored at least six symptoms out of nine in each domain was considered as a positive diagnosis. BMI was calculated from the weight and height of the participants.
The odds ratio (OR) of ADHD was calculated for LCPD against non-LCPD. Logistic regression was used to assess the clinical characteristics and demographics that could be risk factors for LCPD.
Chi-squared test was used to assess the association between ADHD and LCPD. Fisher's exact test was used when the expected cell count was <5. ORs of ADHD and subdiagnoses, as well as 95% confidence intervals, were reported.
Results
Demographics
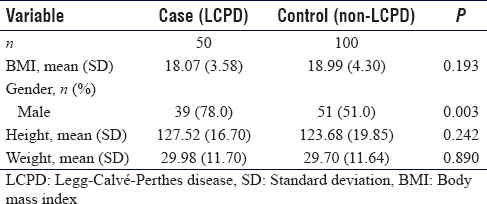
LCPD patients (hereafter referred to as “case group”) were 50 subjects and general population (hereafter referred to as “control group”) were 100 subjects. In the case group, we collected the data from 11 females and 39 males (22% and 78% respectively) with age ranging from 4 to 19 years and a mean age of 9 years. While in the control group, we collected the data from 47 females and 53 males (47% and 53% respectively) with the age range of 4–15 years and a mean age of 8 years.
Legg–Calvé–Perthes disease versus non-Legg–Calvé–Perthes disease
In the case group, we found that it has a significant male predominance (78%).
The average BMI of the case group was 18.07 compared to 18.99 kg/m2 in the control group.
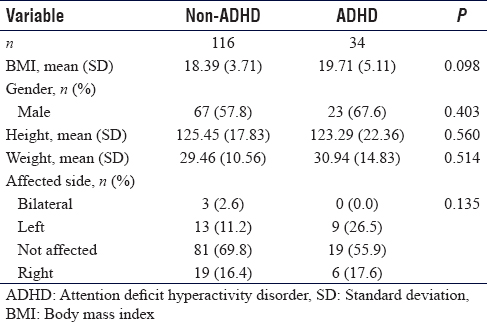
Within the case group, the affected hips were as follows: 3 bilateral (6%); 22 left (44%); and 25 right (50%) [Table - 1] and [Table - 2].
Attention deficit hyperactivity disorder versus non-attention deficit hyperactivity disorder
From the total study population, 34 individuals (22.7%) were diagnosed with ADHD. It was diagnosed in 23 males and 11 females (67.6% and 32.4% respectively). Their average BMI was 19.71 compared to 18.39 in patients with no ADHD diagnosis [Table - 2].
Overall attention deficit hyperactivity disorder diagnosis
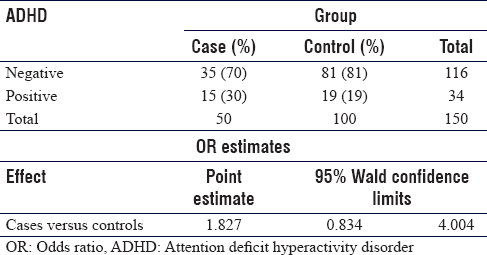
In both groups, 34 children (22.7%) were diagnosed with ADHD, 15 (30%) in the case group and 19 (19%) in the control group. There is no statistically significant difference in ADHD incidence between the case group and the control group (P = 0.1293, OR = 1.827) [Table - 3].
Hyperactive-impulsiveness
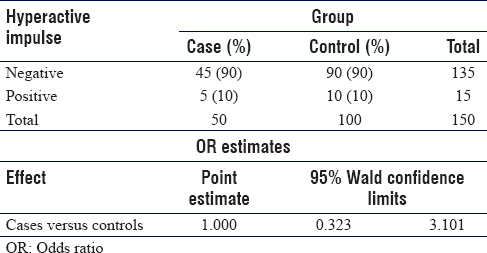
The hyperactive-impulsive subtype of ADHD was found in 15 children (10%) in both groups, 5 (10%) in the case group and 10 (10%) in the control group. There is no difference in the hyperactive-impulsive subtype incidence between the two groups (P > 0.999, OR = 1.000) [Table - 4].
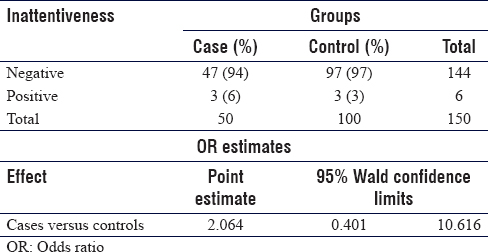
Inattentiveness
The inattentiveness subtype of ADHD was found in 6 children (4%), 3 (6%) in the case group and 3 (3%) in the control group. There is no significant difference in the inattentiveness subtype incidence between the two groups (P = 0.3768, OR = 2.064) [Table - 5].
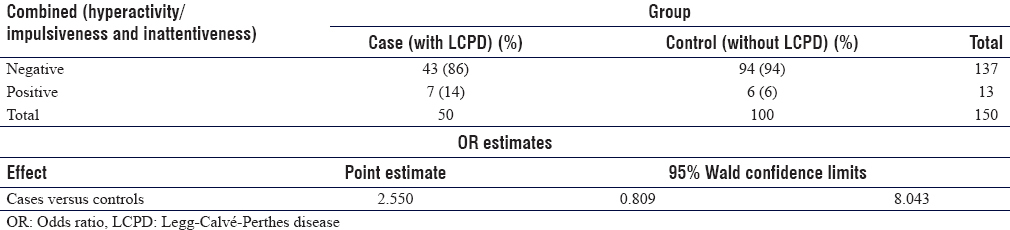
Combined diagnosis
The overall combined subtype of ADHD is 13 cases (8.6%). The incidence of combined subtype in the case group is 7 cases (14%) while 6 (6%) in the control group. There is no significant difference in the combined subtype incidence between both groups (P = 0.1007, OR = 2.550) [Table - 6].
Discussion
The correlation between ADHD and LCPD is not a new one; in fact, this possible relation has been addressed in several studies that have highlighted the increased incidence of ADHD among LCPD patients.[13],[14] For example, in 2014, a study conducted in Sweden by Hailer and Nilsson, which compared 4057 individuals with LCPD to a matched sex, age, and region control group of 40570 individuals without LCPD, reported a 1.5-fold higher risk of ADHD in LCPD group compared to their sex- and age-matched individuals without LCPD.[14] An older study by Loder et al., reported a 33% incidence of ADHD among LCPD patients compared to 3%–5% in normal population, they also suggested a correlation between ADHD and LCPD in regard to certain epidemiological factors, which were similar between the two disorders.[13] However, these two conclusions were different from ours, which showed a difference that was not significant between the two groups (control and case groups) regarding ADHD incidence, although the incidence in our case, group was almost similar to their LCPD patients' incidence (30% vs. 33%) and it was almost 1.5 times higher as it was 30% in the case group compared to 19% in the control group similar to the Swedish study.[13],[14]
On the other hand, we found a study that supports our results showing no significant difference in ADHD incidence between the case group and the control group. This study was conducted in 2014 in Turkey by Türkmen et al., and it stated that the difference in the rate of ADHD was not statistically significant among the three groups studied, which were case group, trauma group, and normal group.[16]
Our results showed a male predominance in the case group (78%), which is strongly consistent with the gender predominance of the reported LCPD demographical studies. A study by Loder et al. reported a male predominance of 81.4%.[2] Another study by Georgiadis et al. reported a similar result of 81.8%.[17]
The current study, also showed an average BMI of 18.07 kg/m2 in case group, compared to 18.99 kg/m2 in the control group, representing a P > 0.19 with no statistically significant difference between the two groups. This result was similar to what Türkmen et al. study reported, in which the average BMI was 20.83 kg/m2 in LCPD group, 19.52 kg/m2 in trauma non-LCPD group, and 19.35 kg/m2 in nontrauma non-LCPD group with no statistically significant difference between the groups.[16]
In this study, the most common site of LCPD is the right hip accounting for 50% of the cases, followed by 44% affected left hip and bilateral disease in 6%. Comparing to Türkmen et al. result, in which right hip was affected in 46% of the cases, left hip was affected in 42% of the cases, and 12% bilateral disease, the results were similar.[16]
In our study, we faced some limitations. Since it is a case–control study, it can have a recalling bias, as our questionnaire asked about past events before the diagnosis of LCPD or the diagnosis of ADHD in older children. Another limitation we had was the small sample size since we had only 50 cases diagnosed with LCPD.
Conclusions
We found that the prevalence of ADHD in LCPD is high (30%), which is comparable to the reported literature but as ADHD was higher than the reported literature in the control group (19%), the difference was statistically insignificant.
Finally, we recommend future researchers studying this area to do a prospective study with multiple centers in different regions in Saudi Arabia, which may increase the sample size and include other variables to be studied, such as, the dietary habits for children, history of trauma, second hand smoking, and the socioeconomic status in the family.
Ethical considerations
Institutional review board's ethical approval was obtained from King Abdullah International Medical Research Center (KAIMRC), and the patient's data were dealt with full confidentiality, the data were kept on a file in a secure location in work PC's only.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Authors' contributions
MAM conceived and designed the study, conducted research, provided research materials, and collected and organized data. SHS analyzed and interpreted data. MAH wrote initial and final draft of the article and provided logistic support. SSM, TAQ, ZSS and BMD has helped in data collection, reviewing the statistics and contributed in writing and editing the paper. All authors have critically reviewed and approved the final draft and are responsible for the content and similarity index of the manuscript.
| 1. | Kim HK. Pathophysiology and new strategies for the treatment of Legg-Calvé-Perthes disease. J Bone Joint Surg Am 2012;94:659-69. [Google Scholar] |
| 2. | Loder RT, Skopelja EN. The epidemiology and demographics of Legg-Calvé-Perthes' disease. ISRN Orthop 2011;2011:504393. [Google Scholar] |
| 3. | American Psychiatric Association. Attention-Deficit/Hyperactivity Disorder. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Washington, DC: American Psychiatric Association; 2013. p. 59. [Google Scholar] |
| 4. | Willcutt EG. The prevalence of DSM-IV attention-deficit/hyperactivity disorder: A meta-analytic review. Neurotherapeutics 2012;9:490-9. [Google Scholar] |
| 5. | Alqahtani MM. Attention-deficit hyperactive disorder in school-aged children in Saudi Arabia. Eur J Pediatr 2010;169:1113-7. [Google Scholar] |
| 6. | Al-Modayfer OA. A pilot study on the prevalence of psychiatric disorders among Saudi children and adolescents: A sample from a selected community in Riyadh city. Arab J Psychiatry 2015;26:184-92. [Google Scholar] |
| 7. | Abu Taleb R, Farheen A. A descriptive study of attention deficit hyperactivity disorder in Sabia city, Saudi Arabia. Int J Cur Res Rev 2013;5:36-41. [Google Scholar] |
| 8. | Homidi MA, Obaidat Y, Hamaidi D. Prevalence of attention deficit and hyperactivity disorder among primary school students in Jeddah city, KSA. Life Sci J 2013;10:280-5. [Google Scholar] |
| 9. | Jenahi E, Khalil MS, Bella H. Prevalence of attention deficit hyperactivity symptoms in female schoolchildren in Saudi Arabia. Ann Saudi Med 2012;32:462-8. [Google Scholar] |
| 10. | Al Hamed JH, Taha AZ, Sabra AA, Bella H. Attention deficit hyperactivity disorder (ADHD) among male primary school children in Dammam, Saudi Arabia: Prevalence and associated factors. J Egypt Public Health Assoc 2008;83:165-82. [Google Scholar] |
| 11. | Alqahtani M. Neurobehavioral outcomes of school-age children born preterm: A preliminary study in the Arabic community. J Pediatr Neonatal Individualized Med 2016;5:e050211. [Google Scholar] |
| 12. | Franke B, Faraone SV, Asherson P, Buitelaar J, Bau CH, Ramos-Quiroga JA, et al. The genetics of attention deficit/hyperactivity disorder in adults, a review. Mol Psychiatry 2012;17:960-87. [Google Scholar] |
| 13. | Loder RT, Schwartz EM, Hensinger RN. Behavioral characteristics of children with Legg-Calvé-Perthes disease. J Pediatr Orthop 1993;13:598-601. [Google Scholar] |
| 14. | Hailer YD, Nilsson O. Legg-Calvé-Perthes disease and the risk of ADHD, depression, and mortality. Acta Orthop 2014;85:501-5. [Google Scholar] |
| 15. | Subcommittee on Attention-Deficit/Hyperactivity Disorder, Steering Committee on Quality Improvement and Management, Wolraich M, Brown L, Brown RT, DuPaul G, et al. ADHD: Clinical practice guideline for the diagnosis, evaluation, and treatment of attention-deficit/hyperactivity disorder in children and adolescents. Pediatrics 2011;128:1007-22. [Google Scholar] |
| 16. | Türkmen I, Poyanlı O, Unay K, Kemah B, Akan K, Ulusan S, et al. Association between attention deficit and hyperactivity disorder and Perthes disease. Acta Orthop Traumatol Turc 2014;48:67-72. [Google Scholar] |
| 17. | Georgiadis AG, Seeley MA, Yellin JL, Sankar WN. The presentation of Legg-Calvé-Perthes disease in females. J Child Orthop 2015;9:243-7. [Google Scholar] |
Fulltext Views
3,153
PDF downloads
377





