Year: 2018, Volume: 2, Issue: 3, July-September
Original Article
Alexander Joeris, Christopher Vannabouathong, Christian Knoll
p.83-112
Original Article
Khalid H Alzahrani, Sohail Bajammal, Abdullah A Alghamdi, Wael Taha, Savithiri Ratnapalan
p.113-120
Original Article
Ghazwan A Hasan, Hayder Q Raheem, Luay M Al-Naser, Reda A Sheta
p.121-125
Original Article
Abdullah A Alturki, Suhail S Alassiri, Mohammed J Alsalman, Ahmad F Afaleh, Fahad H Alhelal, Hanadi M Alqahtani, Ali A Alhandi
p.126-129
Case Report
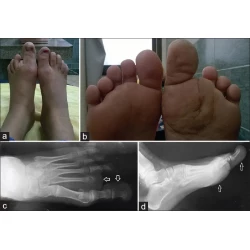
Hala Abdulhady, Tamer A El-Sobky, Nermine S Elsayed, Hossam M Sakr
p.130-134
p.135-136
Letter to Editor
Ganesh Singh Dharmshaktu, Tanuja Pangtey, Shailendra Singh Bhandari
p.137-138